Patients who suffer from psychosis (including schizophrenia, schizoaffective, bipolar, etc.) will experience various symptoms. The symptoms of psychosis can be grouped into three clusters:
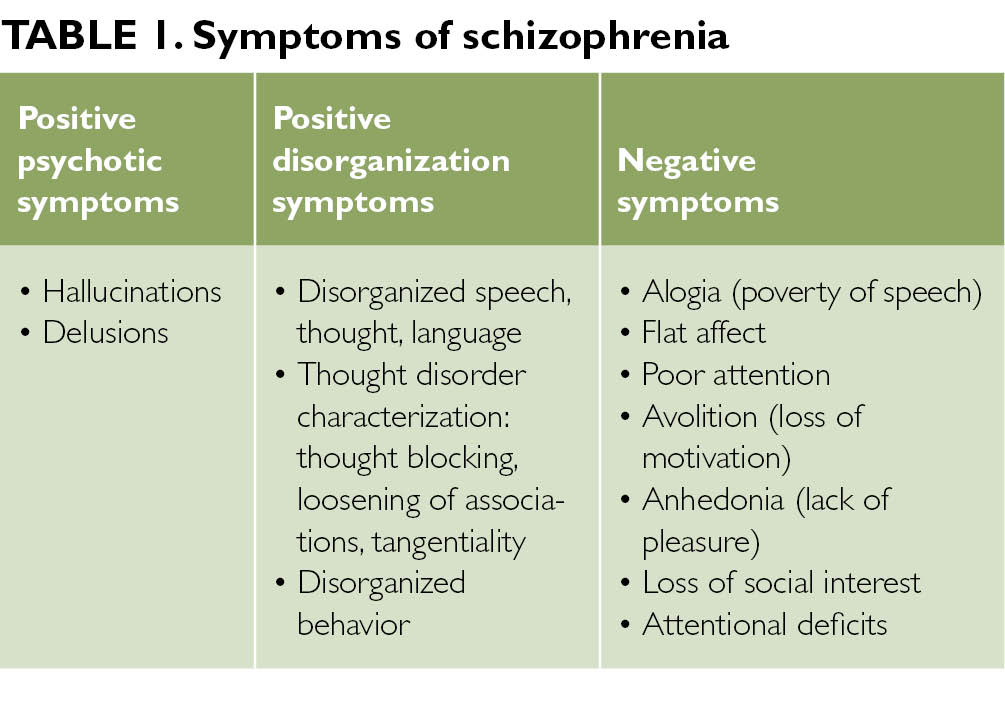
1. Positive symptoms:
i). Hallucinations: A perception-like experience with the clarity and impact of a true perception, but without the external stimulation of the relevant sensory organ, including visual, auditory, tactile, olfactory, gustatory and general somatic hallucination;
ii). Delusions: Fixed beliefs that are not based on reality and are not amenable to change in light of conflicting evidence, including Persecutory Delusions, Referential Delusions, Grandiose Delusions, Erotomanic Delusions, Nihilistic Delusions, Somatic Delusions; Delusion of control (Body control, Thought insertion, Thought withdrawal, Thought broadcasting, Mindreading); Delusional Misidentification Syndromes ( Capgras delusion, Fregoli delusion, Cotard delusion).
2. Cognitive symptoms or disorganized symptoms (e.g. grossly disorganized, bizarre or catatonic behaviors, disorganized thoughts, memory problems, and difficulties with focus and attention).
3. Negative symptoms: Inability to initiate and persist in goal-directed activities or diminished emotional expressiveness, including avolition, alogia, amotivation, physical anergia, anhedonia, asociality, affective flattening, and impoverished thought.
i). Affective flattening: emotional inexpressiveness and apparent unresponsiveness
ii). Alogia: poverty of speech
iii). Asociality: apparent lack of desire for the company of others;
iv). Anhedonia: apparent inability to show or feel pleasure;
v). Avolition: lack of will, spontaneity, and initiative. Some schizophrenic patients show avolition in that they will sit still for long periods of time, seemingly indifferent to their surroundings, and without displaying any interest in work or social activities. In extreme cases, this behavior becomes catatonia
vi): physical anergia: lethargic, at time, unresponsive at times
The outbreak of positive symptoms, which are often the most vivid and conspicuous, is often what brings a person to hospital for psychiatric treatment for the first time. Yet, those positive symptoms are not the most important ones. Negative symptoms in psychosis are actually more pervasive and persistent and have a much greater impact on a patient’s quality of life. As positive symptoms can be quickly spotted, they make illness seem more acute, and they can often be treated with psychotropic agents effectively. On the other hand, research shows negative symptoms are the main reason patients with psychosis cannot live independently, hold jobs, establish personal relationships, and manage everyday social situations. In a seven-year follow-up of patients after a first psychotic break, researchers found that those with the best outcome had the least severe negative symptoms.
One of the challenges in finding the underlying etiology of negative symptoms in schizophrenia stems from the difficulty in distinguishing between primary and secondary negative symptoms. Primary negative symptoms tend to be chronic, frustrating, and extremely debilitating, and are often idiopathic with the “deficit” syndrome. Secondary negative symptoms are iatrogenic, environmental, and might originate secondary to a lot of conditions, related directly or indirectly to the disease under treatment. These included long-term institutionalization, lack of environmental stimuli, poor social support, secondary to positive symptoms, other psychiatric illnesses as depression, and exacerbations of the disease as such and side effects of antipsychotic medications (e.g. TD, EPS, and neuroleptic dysphoria). It’s advised that symptom-targeted pharmacological therapy with psychosocial interventions may offer some effective treatment strategy for ameliorating negative symptoms, and ultimately improving functional outcomes for individuals with schizophrenia.

Mental Status Examination:
- Appearance: Examples of items in the appearance category include body type, posture, poise, clothes, grooming, hair, and nails. Common terms used to describe appearance are healthy, sickly, ill at ease, looks older/younger than stated age, disheveled, childlike, and bizarre. Signs of anxiety are noted: moist hands, perspiring forehead, tense posture and wide eye
- Behavior and Psychomotor Activity: This can include: Mannerisms, tics, gestures, twitches, stereotyped behavior, echopraxia, hyperactivity, agitation, combativeness, flexibility, rigidity, gait, and agility. Take note of movements which can result from drug side effects eg. TD or EPS or tremors. Describe restlessness, wringing of hands, pacing, and other physical manifestations. Note psychomotor retardation or generalized slowing of body movements. Describe any aimless, purposeless activity.
- Attitude towards the Examiner: Cooperative, friendly, attentive, interested, frank, seductive, defensive, contemptuous, perplexed, apathetic, hostile, playful, ingratiating, evasive, or guarded; any number of other adjectives can be used. Record the level of rapport established.
- Speech: can be described in terms of its quantity, rate of production, and quality. Such as: talkative, garrulous, voluble, taciturn, unspontaneous, or normally responsive to cues from the interviewer. Alogia or poverty of speech. Speech can be rapid or slow, pressured (hard to interrupt the pt), hesitant, emotional, dramatic, monotonous, loud, whispered, slurred, staccato, or mumbled. Speech impairments, such as stuttering, are included in this section. Any unusual rhythms (termed dysprosody) or accent should be noted.
- Mood: is defined as a pervasive and sustained emotion that colors the person’s perception of the world. Usually means patient’s self reported mood. Does the patient remark voluntarily about feelings or whether it is necessary to ask the patient how he or she feels? Statements about the patient’s mood should include depth, intensity, duration, and fluctuations. Common adjectives used to describe mood include depressed, despairing, irritable, anxious, angry, expansive, euphoric, empty, guilty, hopeless, futile, self-contemptuous, frightened, and perplexed. Mood can be labile, fluctuating or alternating rapidly between extremes (e.g., laughing loudly and expansively one moment, tearful and despairing the next).
- Affect: Patient’s present emotional responsiveness, inferred from the patient’s facial expression, including the amount and the range of expressive behavior. Quality: Dysphoric, Euthymic (normal) or Elevated/Euphoric in mania, Flat or labile (all over the place), or irritable. Congruency: Affect may or may not be congruent with mood. Range: Affect can be described as within normal range, constricted, blunted, or flat. In the normal range of affect can be variation in facial expression, tone of voice, use of hands, and body movements. When affect is constricted, the range and intensity of expression are reduced. In blunted affect, emotional expression is further reduced. To diagnose flat affect, virtually no signs of affective expression should be present; the patient’s voice should be monotonous and the face should be immobile. Note the patient’s difficulty in initiating, sustaining, or terminating an emotional response. The appropriateness of affect: means appropriateness of the patient’s emotional responses in the context of the subject the patient is discussing. Delusional patients who are describing a delusion of persecution should be angry or frightened about the experiences they believe are happening to them. Inappropriate affect for a quality of response found in some schizophrenia patients, in which the patient’s affect is incongruent with what the patient is saying (e.g., flattened affect when speaking about murderous impulses).
- Perception: Perceptual disturbances, such as hallucinations and illusions, can be experienced in reference to the self or the environment. This can be sometimes inferred also when the patient clearly responds to internal stimuli (and can be described as such). The sensory system involved (e.g., auditory, visual, taste, olfactory, or tactile) and the content of the illusion or the hallucinatory experience should be described. Feelings of depersonalization and derealization (extreme feelings of detachment from the self or the environment) are also part of this section.
- Thought process and thought content: Process refers to the way in which a person puts together ideas and associations, the form in which a person thinks. Process or form of thought can be logical and coherent or completely illogical and even incomprehensible. The patient may have either an overabundance or a poverty of ideas. There may be rapid thinking, which, if carried to the extreme, is called a flight of ideas. A patient may exhibit slow or hesitant thinking. Thought can be vague or empty. – Do the patient’s replies really answer the questions asked? – Does the patient have the capacity for goal-directed thinking? – Are the responses relevant or irrelevant? – Is there a clear cause-and effect relation in the patient’s explanations? – Does the patient have loose associations (e.g., do the ideas expressed seem unrelated and idiosyncratically connected)? Disturbances of thought continuity include statements that are: – tangential, circumstantial, rambling, evasive, or perseverative.
Formal Thought Disorders: Circumstantiality : Overinclusion of trivial or irrelevant details that impede the sense of getting to the point. Tangentiality : In response to a question, the patient gives a reply that is appropriate to the general topic without actually answering the question. Example: – Doctor: “Have you had any trouble sleeping lately?” – Patient: “I usually sleep in my bed, but now I’m sleeping on the sofa.” Derailment : (Synonymous with loose associations) A breakdown in both the logical connection between ideas and the overall sense of goal-directedness. The words make sentences, but the sentences do not make sense. Word Salad (Schizophasia): Incoherent or incomprehensible connections of words or phases. Flight of ideas: A succession of multiple associations so that thoughts seem to move abruptly from idea to idea; often (but not invariably) expressed through rapid, pressured speech. Clang associations: Thoughts are associated by the sound of words rather than by their meaning (e.g., through rhyming, or assonance). Neologism: The invention of new words or phrases or the use of conventional words in idiosyncratic ways. Perseveration: Repetition of out of context of words, phrases, or ideas. Thought blocking : interruption of the train of thought before an idea has been completed; the patient may indicate an inability to recall what was being said or intended to be said.
Content refers to what a person is actually thinking about: ideas, beliefs, preoccupations, obsessions. Disturbances in content of thought include delusions, preoccupations (which may involve the patient’s illness), obsessions, compulsions, phobias, hypochondriacal symptoms, and specific antisocial urges. Does the patient have thoughts of doing self harm? Is there a plan? Note homicidal ideation, intent or plan. Delusions—fixed, false beliefs out of keeping with the patient’s cultural background— may be mood congruent (thoughts that are in keeping with a depressed or elated mood, e.g., a depressed patient thinks he is dying or an elated patient thinks she is the Virgin Mary) or mood incongruent (e.g., an elated patient thinks he has a brain tumor). Describe the content of any delusional system and attempt to evaluate its organization and the patient’s conviction about its validity. • Delusions can be bizarre and may involve beliefs about external control (Thought insertion, withdrawal or broadcasting). Delusions can have themes that are persecutory or paranoid, grandiose, jealous, somatic, guilty, nihilistic, or erotic. Ideas of reference include a person’s belief that the television or radio is speaking to or about him or her. Examples of ideas of influence are beliefs about another person or force controlling some aspect of one’s behavior.
- Cognition/ Sensorium: Level of Alertness and Orientation. Some terms used to describe the patient’s level of consciousness are clouding, somnolence, stupor, coma, lethargy, or alert. Orientation to time, place and person. Cognition: Usually not extensively reported and can be inferred from the interview or reported as ‘intact”. If indicated a miniCog can be done – Orientation – 3 word recall – Concentration – spell WORLD backwards or serial 7s. If impairment is suspected a MMSE and/or a MOCA is most appropriate – These and other bedside tests will test Memory (immediate, recent, long term), Calculations, Fund of knowledge, Abstract reasoning
- Insight and Judgment: there are 6 levels of insight: 1). Complete denial of illness. 2). Slight awareness of being sick and needing help, but denying it at the same time 3). Awareness of being sick but blaming it on others, on external factors, or on organic factors 4). Awareness that illness is caused by something unknown in the patient. 5). Intellectual insight: admission that the patient is ill and that symptoms or failures in social adjustment are caused by the patient’s own particular irrational feelings or disturbances without applying this knowledge to future experiences. 6). True emotional insight: emotional awareness of the motives and feelings within the patient and the important persons in his or her life, which can lead to basic changes in behavior. Judgment: During interview one can assess/infer many aspects of the patient’s capability for social judgment. Does the patient understand the likely outcome of his or her behavior, and is he or she influenced by this understanding? Can the patient predict what he or she would do in imaginary situations (e.g., smelling smoke in a crowded movie theater)? If impaired, then it is a safety issue and therefore it makes this an important aspect of MSE.
Related article for reading:
Assessment of the Awake but Unresponsive Patient https://www.ncbi.nlm.nih.gov/pmc/articles/PMC419301/
Psychiatric interview, history, and mental status examination
https://www.brown.edu/Courses/BI_278/Other/Teaching%20examples/biomed-370/articles/hx_and_ms.pdf
References:
Erhart SM, et al. “Treatment of Schizophrenia Negative Symptoms: Future Prospects,” Schizophrenia Bulletin (April 2006): Vol. 32, No. 2, pp. 234–37.
Kirkpatrick B, et al. “The NIMH-MATRICS Consensus Statement on Negative Symptoms,” Schizophrenia Bulletin (April 2006): Vol. 32, No. 2, pp. 214–219.
Kaplan and Saddock. Synopsis of Psychiatry 10th Ed. Chapt. 7 – Clinical Examination of the Psychiatric Patient
Mitra S, Mahintamani T, Kavoor AR, Nizamie SH. Negative symptoms in schizophrenia. Ind Psychiatry J. 2016;25(2):135–144. doi:10.4103/ipj.ipj_30_15
